Relación entre el realce parenquimatoso de fondo y los distintos subtipos moleculares de cáncer de mama.
Palabras clave:
realce parenquimatoso, poster, seram, subtipos moleculares, cáncer de mama, parénquima peritumoral, RPF, realce parenquimatoso de fondoResumen
Objetivos
INTRODUCCIÓN Y OBJETIVOS
El cáncer de mama es un conjunto de enfermedades diversas con tipos histológicos, presentaciones clínicas y respuestas al tratamiento distintos.
El perfil de expresión génica, basándose en las similitudes genéticas que comparten estos cánceres, proporciona cierta organización estableciendo subtipos moleculares (1,2).
Avances en este campo han conseguido que se clasifique el cáncer de mama en cuatro subtipos moleculares distintos: Luminal A, Luminal B, HER 2, y triple negativo. Son estos subtipos moleculares los que proporcionan a los clínicos un nuevo método para predecir la evolución clínica y los beneficios del tratamiento, independientemente de los factores de riesgo tradicionales, de modo que puedan seleccionar el tratamiento más apropiado para cada paciente y ofrecer un manejo individualizado de su enfermedad (3).
Hasta la fecha, la mayoría de los estudios sobre cáncer de mama se han centrado en la caracterización del tumor en sí mismo. Pero se conoce relativamente poco sobre el significado diagnóstico y pronóstico que posee el parénquima peritumoral en RM.
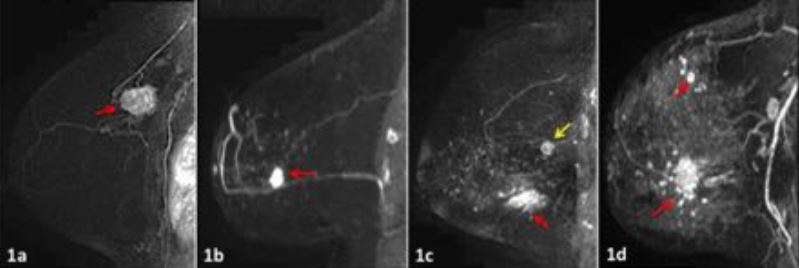
La captación del tejido fibroglandular de la mama en RM se denomina realce parenquimatoso de fondo (RPF) y según su cantidad se clasifica en mínimo, leve, moderado o marcado, siguiendo las recomendaciones de léxico para RM de la quinta edición del sistema BI-RADS® (4).
Descargas
Citas
(1) Perou CM, Sorlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA, et al. Molecular portraits of human breast tumours. Nature 2000 Aug 17;406(6797):747-752.
(2) Sorlie T, Perou CM, Tibshirani R, Aas T, Geisler S, Johnsen H, et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci U S A 2001 Sep 11;98(19):10869-10874.
(3) Lam SW, Jimenez CR, Boven E. Breast cancer classification by proteomic technologies: current state of knowledge. Cancer Treat Rev 2014 Feb;40(1):129-138.
(4) Morris E, Comstock C, Lee C, et al. Magnetic Resonance Imaging. ACR BI-RADS® Atlas, Breast Imaging Reporting and Data System. Reston, VA, American College of Radiology : Reston, VA, American College of Radiology; 2013.
(5) Preibsch H, Wanner L, Bahrs SD, Wietek BM, Siegmann-Luz KC, Oberlecher E, et al. Background parenchymal enhancement in breast MRI before and after neoadjuvant chemotherapy: correlation with tumour response. Eur Radiol 2015 Sep 17.
(6) Kim YJ, Kim SH, Choi BG, Kang BJ, Kim HS, Cha ES, et al. Impact of radiotherapy on background parenchymal enhancement in breast magnetic resonance imaging. Asian Pac J Cancer Prev 2014;15(7):2939-2943.
(7) Chen JH, Yu HJ, Hsu C, Mehta RS, Carpenter PM, Su MY. Background Parenchymal Enhancement of the Contralateral Normal Breast: Association with Tumor Response in Breast Cancer Patients Receiving Neoadjuvant Chemotherapy. Transl Oncol 2015 Jun;8(3):204-209.
(8) Schrading S, Kuhl CK. Breast Cancer: Influence of Taxanes on Response Assessment with Dynamic Contrast-enhanced MR Imaging. Radiology 2015 Dec;277(3):687-696.
(9) Polyak K. Breast cancer: origins and evolution. J Clin Invest 2007 Nov;117(11):3155-3163.
(10) Quail DF, Joyce JA. Microenvironmental regulation of tumor progression and metastasis. Nat Med 2013 Nov;19(11):1423-1437.
(11) Jones EF, Sinha SP, Newitt DC, Klifa C, Kornak J, Park CC, et al. MRI enhancement in stromal tissue surrounding breast tumors: association with recurrence free survival following neoadjuvant chemotherapy. PLoS One 2013 May 7;8(5):e61969.
(12) King V, Brooks JD, Bernstein JL, Reiner AS, Pike MC, Morris EA. Background parenchymal enhancement at breast MR imaging and breast cancer risk. Radiology 2011 Jul;260(1):50-60.
(13) Dontchos BN, Rahbar H, Partridge SC, Korde LA, Lam DL, Scheel JR, et al. Are Qualitative Assessments of Background Parenchymal Enhancement, Amount of Fibroglandular Tissue on MR Images, and Mammographic Density Associated with Breast Cancer Risk? Radiology 2015 Aug;276(2):371-380.
(14) Telegrafo M, Rella L, Stabile Ianora AA, Angelelli G, Moschetta M. Breast MRI background parenchymal enhancement (BPE) correlates with the risk of breast cancer. Magn Reson Imaging 2016 Feb;34(2):173-176.
(15) Morris EA. Diagnostic breast MR imaging: current status and future directions. Radiol Clin North Am 2007 Sep;45(5):863-80, vii.
(16) Soderqvist G, Isaksson E, von Schoultz B, Carlstrom K, Tani E, Skoog L. Proliferation of breast epithelial cells in healthy women during the menstrual cycle. Am J Obstet Gynecol 1997 Jan;176(1 Pt 1):123-128.
(17) Kuhl CK, Bieling HB, Gieseke J, Kreft BP, Sommer T, Lutterbey G, et al. Healthy premenopausal breast parenchyma in dynamic contrast-enhanced MR imaging of the breast: normal contrast medium enhancement and cyclical-phase dependency. Radiology 1997 Apr;203(1):137-144.
(18) Soderqvist G, Isaksson E, von Schoultz B, Carlstrom K, Tani E, Skoog L. Proliferation of breast epithelial cells in healthy women during the menstrual cycle. Am J Obstet Gynecol 1997 Jan;176(1 Pt 1):123-128.
(19) Kim MY, Choi N, Yang JH, Yoo YB, Park KS. Background parenchymal enhancement on breast MRI and mammographic breast density: correlation with tumour characteristics. Clin Radiol 2015 Jul;70(7):706-710.
(20) Uematsu T, Kasami M, Watanabe J. Does the degree of background enhancement in breast MRI affect the detection and staging of breast cancer? Eur Radiol 2011 Nov;21(11):2261-2267.
(21) Baek JE, Kim SH, Lee AW. Background parenchymal enhancement in breast MRIs of breast cancer patients: impact on tumor size estimation. Eur J Radiol 2014 Aug;83(8):1356-1362.
(22) Kim JY, Kim SH, Kim YJ, Kang BJ, An YY, Lee AW, et al. Enhancement parameters on dynamic contrast enhanced breast MRI: do they correlate with prognostic factors and subtypes of breast cancers? Magn Reson Imaging 2015 Jan;33(1):72-80.
(23) Koo HR, Cho N, Song IC, Kim H, Chang JM, Yi A, et al. Correlation of perfusion parameters on dynamic contrast-enhanced MRI with prognostic factors and subtypes of breast cancers. J Magn Reson Imaging 2012 Jul;36(1):145-151.