LOS VENTRÍCULOS:
VIAJE AL FONDO DE LA MENTE
Palabras clave:
LOS VENTRÍCULOS, poster, seram, LCRResumen
Objetivos Docentes
• Ser una herramienta práctica en la evaluación de los ventrículos cerebrales en la práctica diaria.
• Profundizar en el conocimiento anatómico y fisiológico del sistema ventricular.
• Reconocer variantes anatómicas o hallazgos sin trascendencia y revisar las principales entidades patológicas así como las técnicas para su diagnóstico y control a través de casos, con especial atención a la hidrocefalia.
Revisión del tema
Introducción
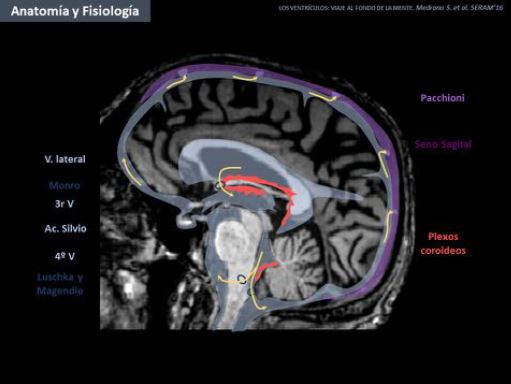
El sistema ventricular otorga protección, flotabilidad y equilibrio químico a las estructuras intracraneales. Mediante este trabajo se pretende ilustrar su anatomía radiológica normal y variante y presentar su espectro patológico así como las técnicas diagnósticas de las que disponemos actualmente para su diagnóstico y control. Se revisan especialmente las alteraciones en la presión del LCR (hidrocefalia e hipotensión licuoral), y se muestran algunas claves para el diagnóstico diferencial entre la hidrocefalia y la atrofia. Se revisan más brevemente otras entidades (congénitas, degenerativas, causas de hemorragia intraventricular, ventriculitis, tumores y cambios posquirúrgicos).
Descargas
Citas
Rigamonti D. Adult Hydrocephalus. (Rigamonti D, ed.). Cambridge: Cambridge University Press; 2014. doi:10.1017/CBO9781139382816.
Crisan E. et al. Ventricles of the Brain: Overview, Gross Anatomy, Microscopic Anatomy. Medscape. http://emedicine.medscape.com/article/1923254-overview. Published 2013. Accessed March 6, 2016.
Wanifuchi H, Shimizu T, Maruyama T. Age-related changes in the proportion of intracranial cerebrospinal fluid space measured using volumetric computerized tomography scanning. J Neurosurg. 2002;97(3):607-610. doi:10.3171/jns.2002.97.3.0607.
Kaye JA1, DeCarli C, Luxenberg JS RS. The significance of age-related enlargement of the cerebral ventricles in healthy men and women measured by quantitative computed X-ray tomography. J Am Geriatr Soc. 1992;40(3):225-231. http://www.ncbi.nlm.nih.gov/pubmed/1538040.
Singh BR, Gajbe U, Agrawal A, Reddy YA, Bhartiya S. Ventricles of brain: A morphometric study by computerized tomography. Int J Med Res Heal Sci. 2014;3(2):381.
doi:10.5958/j.2319-5886.3.2.079.
EVANS WA. AN ENCEPHALOGRAPHIC RATIO FOR ESTIMATING VENTRICULAR ENLARGEMENT AND CEREBRAL ATROPHY. Arch Neurol Psychiatry. 1942;47(6):931. doi:10.1001/archneurpsyc.1942.02290060069004.
C. G. Measurements of the normal ventricular system and hemispheric sulci of 100 adults with computed tomography. Neuroradiology. 1977;14(4):183-192.
Toma AK, Holl E, Kitchen ND, Watkins LD. Evans’ index revisited: the need for an alternative in normal pressure hydrocephalus. Neurosurgery. 2011;68(4):939-944. doi:10.1227/NEU.0b013e318208f5e0.
Doraiswamy PM, Patterson L, Na C, et al. Bicaudate index on magnetic resonance imaging: effects of normal aging. J Geriatr Psychiatry Neurol. 7(1):13-17.
http://www.ncbi.nlm.nih.gov/pubmed/8192824. Accessed March 4, 2016.
Ho VB, Chuang HS, Rovira MJ, Koo B. Juvenile Huntington disease: CT and MR features. Am J Neuroradiol. 1995;16(7):1405-1412.
Virhammar J, Laurell K, Cesarini KG, Larsson E-M. Preoperative Prognostic Value of MRI Findings in 108 Patients with Idiopathic Normal Pressure Hydrocephalus. AJNR Am J Neuroradiol. 2014;58:1-8. doi:10.3174/ajnr.A4046.
Virhammar J, Laurell K, Cesarini KG, Larsson E-M. The callosal angle measured on MRI as a predictor of outcome in idiopathic normal-pressure hydrocephalus. J Neurosurg. 2014;120(1):178-184. doi:10.3171/2013.8.JNS13575.
Nestor SM, Rupsingh R, Borrie M, et al. Ventricular enlargement as a possible measure of Alzheimer’s disease progression validated using the Alzheimer's disease neuroimaging initiative database. Brain. 2008;131(Pt 9):2443-2454. doi:10.1093/brain/awn146.
Bakshi R, Caruthers SD, Janardhan V, Wasay M. Intraventricular CSF pulsation artifact on fast fluid-attenuated inversion-recovery MR images: analysis of 100 consecutive normal studies. AJNR Am J Neuroradiol. 2000;21(3):503-508. http://www.ncbi.nlm.nih.gov/pubmed/10730642. Accessed March 8, 2016.
Whitehead MT, Oh C, Raju A, Choudhri AF. Physiologic pineal region, choroid plexus, and dural calcifications in the first decade of life. AJNR Am J Neuroradiol. 2015;36(3):575-580.
doi:10.3174/ajnr.A4153.
Hosseinzadeh K, Luo J, Borhani A, Hill L. Non-visualisation of cavum septi pellucidi: implication in prenatal diagnosis? Insights Imaging. 2013;4(3):357-367.
doi:10.1007/s13244-013-0244-x.
Epelman M, Daneman A, Blaser SI, et al. Differential diagnosis of intracranial cystic lesions at head US: correlation with CT and MR imaging. Radiographics. 26(1):173-196.
doi:10.1148/rg.261055033.
Sze G, de Armond SJ, Brant-Zawadzki M, Davis RL, Norman D, Newton TH. Foci of MRI signal (pseudo lesions) anterior to the frontal horns: Histologic correlations of a normal finding. Am J Roentgenol. 1986;147(2):331-337. doi:10.2214/ajr.147.2.331.
Dormont D, Seidenwurm DJ, Expert Panel on Neurologic Imaging, American College of Radiology. Dementia and movement disorders. AJNR Am J Neuroradiol. 2008;29(1):204-206.
http://www.ncbi.nlm.nih.gov/pubmed/18192345. Accessed March 4, 2016.
Pagani E, Rocca MA, Gallo A, et al. Regional brain atrophy evolves differently in patients with multiple sclerosis according to clinical phenotype. AJNR Am J Neuroradiol. 2005;26(2):341-346. http://www.ncbi.nlm.nih.gov/pubmed/15709132. Accessed March 4, 2016.
de la Monte SM. Disproportionate atrophy of cerebral white matter in chronic alcoholics. Arch Neurol. 1988;45(9):990-992. http://www.ncbi.nlm.nih.gov/pubmed/3415529. Accessed March 4, 2016.
ADAMS RD, FISHER CM, HAKIM S, OJEMANN RG, SWEET WH. SYMPTOMATIC OCCULT HYDROCEPHALUS WITH "NORMAL" CEREBROSPINAL-FLUID PRESSURE.A
TREATABLE SYNDROME. N Engl J Med. 1965;273:117-126. doi:10.1056/NEJM196507152730301.
Marmarou A, Black P, Bergsneider M, Klinge P, Relkin N, International NPH Consultant Group. Guidelines for management of idiopathic normal pressure hydrocephalus: progress to date. Acta Neurochir Suppl. 2005;95:237-240. http://www.ncbi.nlm.nih.gov/pubmed/16463856. Accessed March 5, 2016.
Klinge P, Hellström P, Tans J, Wikkelsø C. One-year outcome in the European multicentre study on iNPH. Acta Neurol Scand. 2012;126(3):145-153. doi:10.1111/j.1600-0404.2012.01676.x.
Edwards RJ, Dombrowski SM, Luciano MG, Pople IK. Chronic hydrocephalus in adults. Brain Pathol. 2004;14(3):325-336. http://www.ncbi.nlm.nih.gov/pubmed/15446589. Accessed March 6, 2016.
Johnston M, Papaiconomou C. Cerebrospinal fluid transport: a lymphatic perspective. News Physiol Sci. 2002;17:227-230. http://www.ncbi.nlm.nih.gov/pubmed/12433975. Accessed March 4, 2016.
Miyakoshi A, Kohno M, Nagata O, Sora S, Sato H. Hydrocephalus associated with vestibular schwannomas: perioperative changes in cerebrospinal fluid. Acta Neurochir (Wien).
;155(7):1271-1276. doi:10.1007/s00701-013-1742-9.
Bech RA, Waldemar G, Gjerris F, Klinken L, Juhler M. Shunting effects in patients with idiopathic normal pressure hydrocephalus; correlation with cerebral and leptomeningeal biopsy findings. Acta Neurochir (Wien). 1999;141(6):633-639. http://www.ncbi.nlm.nih.gov/pubmed/10929729. Accessed March 4, 2016.
Bech RA, Juhler M, Waldemar G, Klinken L GF. Frontal brain and leptomeningeal biopsy specimens correlated with cerebrospinal fluid outflow resistance and B-wave activity in patients suspected of normal-pressure hydrocephalus. Neurosurgery. 1997;40(3):497-502.
Greitz D. Radiological assessment of hydrocephalus: new theories and implications for therapy. Neurosurg Rev. 2004;27(3):145-165; discussion 166-167. doi:10.1007/s10143-004-0326-9.
Bateman GA. The pathophysiology of idiopathic normal pressure hydrocephalus: Cerebral ischemia or altered venous hemodynamics? Am J Neuroradiol. 2008;29(1):198-203.
doi:10.3174/ajnr.A0739.
Jaraj D, Agerskov S, Rabiei K, et al. Vascular factors in suspected normal pressure hydrocephalus: A population-based study. Neurology. 2016;86(7):592-599.
doi:10.1212/WNL.0000000000002369.
Graff-Radford NR. Is normal pressure hydrocephalus becoming less idiopathic? Neurology. 2016;86(7):588-589. doi:10.1212/WNL.0000000000002377.
Bradley WG Jr, Whittemore AR, Watanabe AS, Davis SJ, Teresi LM HM. Association of deep white matter infarction with chronic communicating hydrocephalus: implications regarding the possible origin of normal-pressure hydrocephalus. AJNR Am J Neuroradiol. 1991;12(1):31-39.
Krauss JK, Regel JP, Vach W, Orszagh M, Jüngling FD, Bohus M DD. White matter lesions in patients with idiopathic normal pressure hydrocephalus and in an age-matched control group: a comparative study. Neurosurgery. 1997;40(3):495-496.
Krauss JK, Droste DW, Vach W, Regel JP, Orszagh M, Borremans JJ, Tietz A SW. Cerebrospinal fluid shunting in idiopathic normal-pressure hydrocephalus of the elderly: effect of periventricular and deep white matter lesions. Neurosurgery. 1996;39(292-9).
Boon AJ, Tans JT, Delwel EJ, Egeler-Peerdeman SM, Hanlo PW, Wurzer HA HJ. Dutch Normal-Pressure Hydrocephalus Study: the role of cerebrovascular disease. J Neurosurg.
;90(2):221-226.
Hashimoto M, Ishikawa M, Mori E, Kuwana N, Study of INPH on neurological improvement (SINPHONI). Diagnosis of idiopathic normal pressure hydrocephalus is supported by MRI-based scheme: a prospective cohort study. Cerebrospinal Fluid Res. 2010;7:18. doi:10.1186/1743-8454-7-18.
Bradley WG. CSF Flow in the Brain in the Context of Normal Pressure Hydrocephalus. AJNR Am J Neuroradiol. 2015. doi:10.3174/ajnr.A4124.
Ringstad G, Emblem KE, Geier O, Alperin N, Eide PK. Aqueductal Stroke Volume: Comparisons with Intracranial Pressure Scores in Idiopathic Normal Pressure Hydrocephalus. Am J Neuroradiol. 2015;36(9):1623-1630. doi:10.3174/ajnr.A4340.
Bradley C, Atkinson J. Neuroradlology Normal-Pressure with Cerebrospinal at MR Imaging ’. Radiology. 1996;198:523-529.
Sherman JL, Citrin CM. Magnetic resonance demonstration of normal CSF flow. AJNR Am J Neuroradiol. 7(1):3-6. http://www.ncbi.nlm.nih.gov/pubmed/3082142. Accessed March 8, 2016.
Lenfeldt N, Hansson W, Larsson A, Birgander R, Eklund A, Malm J. Three-day CSF drainage barely reduces ventricular size in normal pressure hydrocephalus. Neurology. 2012;79(3):237-242. doi:10.1212/WNL.0b013e31825fdf8a.
Bradley WM QR. Hydrocephalus and cerebrospinal fluid flow. In: Stark DD BW, ed. Magnetic Resonance Imaging. 3rd ed. St. Louis: Mosby; 1999:1483-1507.
Ulug AM, Truong TN, Filippi CG, et al. Diffusion Imaging in Obstructive Hydrocephalus.
Kazunari Ishii Tomonori Kanda Aya Harada Naokazu Miyamoto Tetsuro Kawaguchi Kenichi Shimada Shingo Ohkawa Takafumi Uemura Toshiki Yoshikawa Etsuro Mori N. Clinical impact of the callosal angle in the diagnosis of idiopathic normal pressure hydrocephalus. Eur Radiol. 2008;18:2678-2683. doi:10.1007/s00330-008-1044-4.
Kitagaki H, Mori E, Ishii K, Yamaji S, Hirono N, Imamura T. CSF spaces in idiopathic normal pressure hydrocephalus: Morphology and volumetry. Am J Neuroradiol. 1998;19(7):1277-1284.
Scollato A, Tenenbaum R, Bahl G, Celerini M, Salani B, Di Lorenzo N. Changes in aqueductal CSF stroke volume and progression of symptoms in patients with unshunted idiopathic normal pressure hydrocephalus. Am J Neuroradiol. 2008;29(1):192-197. doi:10.3174/ajnr.A0785.
Tullberg M, Ziegelitz D, Ribbelin S, Ekholm S. White matter diffusion is higher in Binswanger disease than in idiopathic normal pressure hydrocephalus. Acta Neurol Scand. 2009;120(4):226-234. doi:10.1111/j.1600-0404.2009.01165.x.
Tullberg M, Hultin L, Ekholm S, Månsson J-E, Fredman P, Wikkelsø C. White matter changes in normal pressure hydrocephalus and Binswanger disease: specificity, predictive value and correlations to axonal degeneration and demyelination. Acta Neurol Scand. 2002;105(6):417-426. http://www.ncbi.nlm.nih.gov/pubmed/12027829. Accessed March 4, 2016.
Kiefer M, Eymann R, Steudel WI. [LOVA hydrocephalus - a new entity of chronic hydrocephalus]. Nervenarzt. 2002;73(10):972-981. doi:10.1007/s00115-002-1389-x.
Cowan JA, McGirt MJ, Woodworth G, Rigamonti D, Williams MA. The syndrome of hydrocephalus in young and middle-aged adults (SHYMA). Neurol Res. 2005;27(5):540-547.
doi:10.1179/016164105X17242.
Schievink WI. Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. JAMA. 2006;295(19):2286-2296. doi:10.1001/jama.295.19.2286.
Lay CM. Low Cerebrospinal Fluid Pressure Headache. Curr Treat Options Neurol. 2002;4(5):357-363. http://www.ncbi.nlm.nih.gov/pubmed/12162924. Accessed March 5, 2016.
Lasater GM. Primary intracranial hypotension. The low spinal fluid pressure syndrome. Headache. 1970;10(2):63-66. http://www.ncbi.nlm.nih.gov/pubmed/5423327. Accessed March 5, 2016.
Schievink WI. Misdiagnosis of spontaneous intracranial hypotension. Arch Neurol. 2003;60(12):1713-1718. doi:10.1001/archneur.60.12.1713.
Bakshi R, Mechtler LL, Kamran S, et al. MRI findings in lumbar puncture headache syndrome: abnormal dural-meningeal and dural venous sinus enhancement. Clin Imaging. 23(2):73-76. http://www.ncbi.nlm.nih.gov/pubmed/10416079. Accessed March 5, 2016.
Alvarez-Linera J, Escribano J, Benito-León J, Porta-Etessam J, Rovira A. Pituitary enlargement in patients with intracranial hypotension syndrome. Neurology. 2000;55(12):1895-1897.
http://www.ncbi.nlm.nih.gov/pubmed/11134390. Accessed March 5, 2016.
Mokri B. Spontaneous Intracranial Hypotension. Continuum (Minneap Minn). 2015;21(4 Headache):1086-1108. doi:10.1212/CON.0000000000000193. 60. Osborn AG, Preece MT. Intracranial cysts: radiologic-pathologic correlation and imaging approach. Radiology. 2006;239(3):650-664. doi:10.1148/radiol.2393050823.
Smith AB, Smirniotopoulos JG, Horkanyne-Szakaly I. From the radiologic pathology archives: intraventricular neoplasms: radiologic-pathologic correlation. Radiographics. 33(1):21-43.
doi:10.1148/rg.331125192.
Jelinek J, Smirniotopoulos JG, Parisi JE, Kanzer M. Lateral ventricular neoplasms of the brain: differential diagnosis based on clinical, CT, and MR findings. Am J Neuroradiol. 1990;11(3):567-574.
Darby DG, Donnan GA, Saling MA, Walsh KW, Bladin PF. Primary intraventricular hemorrhage: clinical and neuropsychological findings in a prospective stroke series. Neurology. 1988;38(1):68-75. http://www.ncbi.nlm.nih.gov/pubmed/3257294. Accessed March 6, 2016.
Flint AC, Roebken A, Singh V. Primary intraventricular hemorrhage: yield of diagnostic angiography and clinical outcome. Neurocrit Care. 2008;8(3):330-336. doi:10.1007/s12028-008-9070-2.
Martí-Fàbregas J, Piles S, Guardia E, Martí-Vilalta JL. Spontaneous primary intraventricular hemorrhage: clinical data, etiology and outcome. J Neurol. 1999;246(4):287-291.
http://www.ncbi.nlm.nih.gov/pubmed/10367697. Accessed March 6, 2016.
Passero S, Ulivelli M, Reale F. Primary intraventricular haemorrhage in adults. Acta Neurol Scand. 2002;105(2):115-119. http://www.ncbi.nlm.nih.gov/pubmed/11903121. Accessed March 6, 2016.
Hernalsteen D, Dignac A, Oppenheim C, et al. Hyperacute intraventricular hemorrhage: detection and characterization, a comparison between 5 MRI sequences. J Neuroradiol. 2007;34(1):42-48. doi:10.1016/j.neurad.2007.01.001.
Kanamalla US, Ibarra RA, Jinkins JR. Imaging of cranial meningitis and ventriculitis. Neuroimaging Clin N Am. 2000;10(2):309-331. http://www.ncbi.nlm.nih.gov/pubmed/10775954.
Accessed March 9, 2016.
Fujikawa A, Tsuchiya K, Honya K, Nitatori T. Comparison of MRI sequences to detect ventriculitis. AJR Am J Roentgenol. 2006;187(4):1048-1053. doi:10.2214/AJR.04.1923.
Pezzullo JA, Tung GA, Mudigonda S, Rogg JM. Diffusion-weighted MR imaging of pyogenic ventriculitis. AJR Am J Roentgenol. 2003;180(1):71-75. doi:10.2214/ajr.180.1.1800071.
Mohan S, Jain KK, Arabi M, Shah G V. Imaging of meningitis and ventriculitis. Neuroimaging Clin N Am. 2012;22(4):557-583. doi:10.1016/j.nic.2012.04.003.
Browd SR, Ragel BT, Gottfried ON, Kestle JRW. Failure of cerebrospinal fluid shunts: part I: Obstruction and mechanical failure. Pediatr Neurol. 2006;34(2):83-92.
doi:10.1016/j.pediatrneurol.2005.05.020.
Goeser CD, McLeary MS, Young LW. Diagnostic imaging of ventriculoperitoneal shunt malfunctions and complications. Radiographics. 18(3):635-651. doi:10.1148/radiographics.18.3.9599388.
Wallace AN, McConathy Christine Menias Sanjeev Bhalla Franz J Wippold II Wallace AN JO, Ii WF. Imaging Evaluation of CSF Shunts N e u r o r a d io l og y/ H e a d a n d N e c k I m ag i ng @BULLET R ev i ew. AJR. 2014;202:38-53. doi:10.2214/AJR.12.10270.