RESULTADOS A CORTO PLAZO DE LA CORRELACIÓN CLÍNICO RADIOLÓGICA MEDIANTE RM DE LA TÉCNICA AMIC PARA EL TRATAMIENTO DE LESIONES CONDRALES DE LA RODILLA.
Palabras clave:
TÉCNICA AMIC, poster, seram, LESIONES CONDRALES DE LA RODILLAResumen
Objetivos
INTRODUCCIÓN:
La articulación femoropatelar es compleja y está sometida a fuerzas axiales y de cizallamiento. Los defectos condrales de la misma están asociados con Frecuencia a una presión femoropatelar anormal tal como la compresión lateral o la posición lateral excesiva de la rótula en la tróclea [2,3]. Los defectos del
cartílago rotuliano son frecuentes especialmente en los atletas y jóvenes, los cuales sufren dolor, bloqueo e hinchazón.
Material y métodos
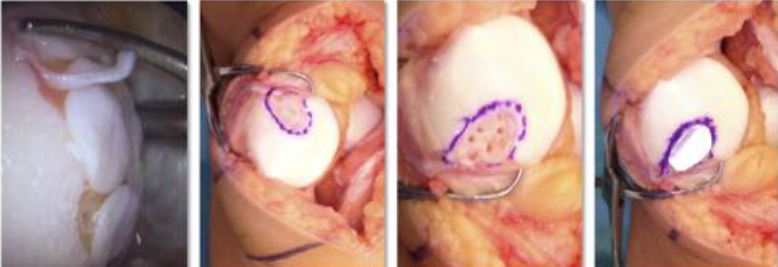
Nueve pacientes entre 24 y 62 años con uno o más defectos condrales focales rotulianos grado III-IV según la escala de Outerbridge, (3 defectos grado III y 6 grado IV), entre 10 y 20 mm de diámetro, fueron tratados mediante la técnica AMIC en nuestra institución entre enero del 2014 a mayo del 2015.
Los criterios de exclusión fueron: edad menor de 15 y mayores de 50 años, la mala alineación femoropatelar o tibio-femoral y los pacientes con lesiones condrales en el fémur, la tibia o tróclea.
Descargas
Citas
Dhollander A, Moens K, Van der Maas J, Verdonk P, Almqvist KF, Victor J. Treatment of patellofemoral cartilage defects in the knee by autologous matrix-induced
chondrogenesis (AMIC). Acta Orthop Belg. 2014 Jun;80(2):251-9. PMID: 25090800
Niemeyer P, Steinwachs M, erggelet C, Kreuz PC, Kraft n, Kostler W, Mehlhorn A, Sudkamp nP. Autologous chondrocyte implantation for the treatment of retropatellar cartilage defects : clinical results referred to defect localisation. Arch Orthop Trauma Surg 2008 ; 128 : 1223-1231.
Pascual-Garrido C, Slabaugh MA, l’Heureux DR, Friel nA, Cole BJ. Recommendations and treatment outcomes for patellofemoral articular cartilage defects with autologous chondrocyte implantation: prospective evaluation at average 4-year follow-up. Am J Sports Med 2009 ; 37 : 33-41.
Differences in patellofemoral joint cartilage material properties and their significance to the etiology of cartilage surface fibrillation. Froimson MI, Ratcliffe A, Gardner TR, Mow VC. Osteoarthritis Cartilage. 1997 Nov;5(6):377-86. PMID: 9536286 http://www.ncbi.nlm.nih.gov/pubmed/9536286
Widuchowski W, Widuchowski J, Trzaska T. Articular cartilage defects: study of 25,124 knee arthroscopies. Knee. 2007;14(3):177-182
Flanigan DC, Harris JD, Trinh TQ, Siston RA, Brophy RH. Prevalence of chondral defects in athletes’ knees: a systematic review. Med Sci Sports Exerc. 2010;42(10):1795-1801.
Gomoll AH, Farr J, Gillogly SD, Kercher J, Minas T. Surgical management of articular cartilage defects of the knee. J Bone Joint Surg Am. 2010;92:2470-2490
Moseley JB Jr, Anderson AF, Browne Je, Mandel - baum BR, Micheli lJ, Fu F, erggelet C. long-term durability of autologous chondrocyte implantation: a multicenter, observational study in US patients. Am J Sports Med 2010 ; 38 : 238-246.
Peterson l, Vasiliadis HS, Brittberg M, lindahl A. Autologous chondrocyte implantation : long-term followup. Am J Sports Med 2010; 38 : 1117-1124.
Joshi N, Reverte-Vinaixa M, Díaz-Ferreiro EW, Dominguez-Oronoz R. Synthetic resorbable scaffolds for the treatment of isolated patellofemoral cartilage defects in young patients: magnetic resonance imaging and clinical evaluation. Am J Sports Med 2012;40:1289–95.
Gobbi A, Karnatzikos G, Sankineani SR. One-step surgery with multipotent stem cells for the treatment of large full-thickness chondral defects of the knee. Am J Sports Med. 2014 Mar;42(3):648-57
Gudas R, Gudaite A, Mickevicius T, Masiulis N, Simonaityte R, Cekanauskas E, Skurvydas A. Comparison of osteochondral autologous transplantation, microfracture, or debridement techniques in articular cartilage lesions associated with anterior cruciate ligament injury: a prospective study with a 3-year follow-up. Arthroscopy. 2013 Jan;29(1):89-97
Lynch TS, Patel RM, Benedick A, Amin NH, Jones MH, Miniaci A. Systematic Review of Autogenous Osteochondral Transplant Outcomes. Arthroscopy. 2015
Apr;31(4):746-754.
Kon E, Roffi A, Filardo G, Tesei G, Marcacci M. Scaffold-Based Cartilage Treatments: With or Without Cells? A Systematic Review of Preclinical and Clinical Evidence. Arthroscopy. 2015 Apr;31(4):767-775
LaPorta TF, Richter A, Sgaglione NA, Grande DA. Clinical relevance of scaffolds for cartilage engineering. Orthop Clin North Am. 2012 Apr;43(2):245-54
Anderson JA, Little D, Toth AP, Moorman CT 3rd, Tucker BS, Ciccotti MG, Guilak F. Stem cell therapies for knee cartilage repair: the current status of preclinical and clinical studies. Am J Sports Med. 2014 Sep;42(9):2253-61.
Bark S, Piontek T, Behrens P, Mkalaluh S, Varoga D, Gille J. Enhanced microfracture techniques in cartilage knee surgery: Fact or fiction?. World J Orthop.
Sep 18;5(4):444-9.
Lee YHD , Suzer F, and Thermann H. Autologous Matrix-Induced Chondrogenesis in the Knee: A Review. Cartilage. 2014, Vol. 5(3) 145–153.
Benthien JP, Behrens P. Autologous matrix-induced chondrogenesis (AMIC) combining microfracturing and a collagen i/iii matrix for articular cartilage resurfacing. Cartilage 2010 ; 1 : 65-68.
Yun Sun Choi, Hollis G. Potter, and Tong Jin Chun. MR Imaging of Cartilage Repair in the Knee and Ankle. RadioGraphics 2008 28:4, 1043-1059
Ware Jr JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992;30:473–83.
Barber FA, Dockery WD. A computed tomography scan assessment of synthetic multiphase polymer scaffolds used for osteochondral defect repair. Arthroscopy. 2011;27(1):60-64.
Carmont MR, Carey-Smith R, Saithna A, Dhillon M, Thompson P, Spalding T. Delayed incorporation of a TruFit plug: perseverance is recommended. Arthroscopy. 2009;25(7):810-814
Marlovits S, Singer P, Zeller P, Mandl I, Haller J, Trattnig S. Magnetic resonance observation of cartilage repair tissue (MOCART) for the evaluation of autologous chondrocyte transplantation: determination of interobserver variability and correlation to clinical outcome after 2 years. Eur J Radiol. 2006;57(1):16-23
Marlovits S, Striessnig G, Resinger CT, et al. Definition of pertinent parameters for the evaluation of articular cartilage repair tissue with high-resolution magnetic resonance imaging. Eur J Radiol 2004; 52(3):310–319.
Trattnig S, Millington SA, Szo Ali Guermazi, Frank W. Roemer, Hamza Alizai, Carl S. Winalski, Goetz Welsch, Mats Brittberg, and Siegfried Trattnig
molanyi P, Marlovits S. MR imaging of osteochondral grafts and autologous chondrocyte implantation. Eur Radiol 2007; 17(1):103–118.
Ali Guermazi, Frank W. Roemer, Hamza Alizai, Carl S. Winalski, Goetz Welsch, Mats Brittberg, and Siegfried Trattnig. State of the Art: MR Imaging after Knee Cartilage Repair Surgery. Radiology 2015 277:1, 23-43