Valoración pronóstica de los factores radio-patológicos del cáncer de mama triple negativo y la respuesta a la quimioterapia neoadyuvante.
Palabras clave:
factores radio-patológicos, poster, seram, cáncer de mama, triple negativo, quimioterapia, tumores triple negativo, TN, CMResumen
Objetivos
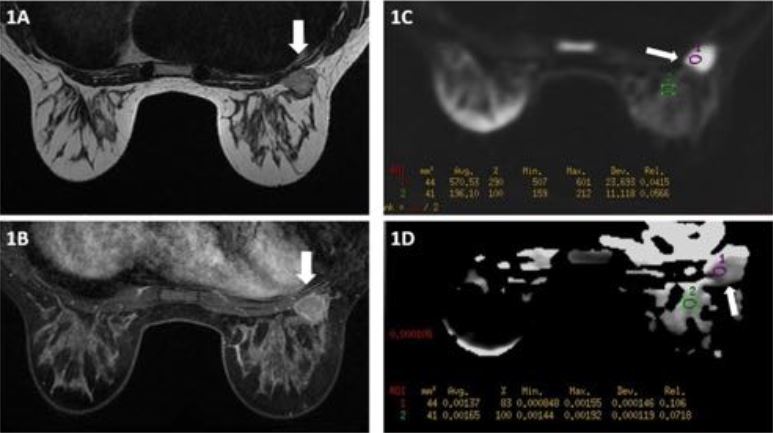
Los tumores triple negativo (TN) son un subgrupo de cáncer de mama (CM) que no expresa receptores hormonales ni el receptor 2 de crecimiento epidérmico humano (HER2). Son tumores agresivos con un alto índice mitótico y alto grado histológico. La carencia de un factor oncogénico dominante limita las opciones terapéuticas al uso de quimioterapia. La resonancia magnética (RM) es la técnica más sensible para la detección de estos tumores y para controlar la respuesta a la quimioterapia (QT), al ser más objetiva en la valoración del tamaño, el cambio morfológico tumoral (reducción concéntrica, fragmentada o mixta), la presencia de necrosis intralesional, intensidad de realce y la morfología de la curva.
Los objetivos de nuestro estudio son: Analizar el pronóstico de las pacientes en función de factores radiológicos valorados mediante RM y anatomo-patológicos de los tumores TN. Y analizar la respuesta radiológica mediante RM y patológica a la QT.
Material y métodos
Se han revisado retrospectivamente todas las RM de mama realizadas en nuestro centro desde el año 2007 al 2014 para recopilar aquellas pacientes con CM TN.
-Criterios de inclusión: RM de estadificación de CM o de seguimiento de CM TN; subtipo molecular TN confirmado con inmunohistoquímica.
-Criterios de exclusión: RM no valorable por problemas técnicos o personales; RM de control posterior a quimioterapia neoadyuvante sin estudio de RM pretratamiento; no valoración de HER2.
Descargas
Citas
Dogan BE, Turnbull LW. Imaging of triple-negative breast cancer. Ann Oncol. 2012; 23 Suppl 6:vi23-9.
Comanescu M, Bussolati G. Cancer stem cells biomarkers in triple negative invasive carcinoma of the breast and associated in situ lesions. Rom J Morphol. 2014;55(2 Suppl):569-74.
Schmadeka R, Harmon BE, Singh M. Triple-negative breast carcinoma. Current and emerging concepts. Am J Clin Pathol. 2014; 141:462-77.
Uematsu T, Kasami M, Yuen S. Triple-negative breast cancer: correlation between MR imaging and pathologic findings. Radiology. 2009; 250:638-47.
Marcos de Paz LM, Tejerina A, Arranz ML, Calvo de Juan V. Resonancia magnética de mama: cambios en la imagen del cáncer tratado con neoadyuvancia. Correlación con subtipos moleculares. Radiología. 2011.
Lin NU, Claus E, Sohl J, Razzak AR, Arnaout A, Winer EP. Sites of distant recurrence and clinical outcomes in patients with metastatic triple negative breast cancer: high incidence of central nervous system metastases. Cancer. 2008;113:2638-45.
Yagata H, Kajiura Y, Yamauchi H. Current strategy for triple-negative breast cancer: appropiate combination of surgery, radiation, and chemotherapy. Breast Cancer. 2011; 18:165-73.
Padhani AR, Hayes C, Assersohn L, Powles T, Mackris A, Suckling J, et al. Prediction of clinic pathologic response of breast cancer to primary chemotherapy at contrast enhanced MR imaging: initial clinical results. Radiology 2006; 239:361-74.
Kim MJ, Kim EK, Park S, Moon HJ, Kim SI, Park BW. Evaluation with 3.0-T MR imaging: predicting the pathological response of triple-negative breast cancer treated with anthracycline and taxane neoadjuvant chemotherapy. Acta Radiol. 2015; 56(9):1069-77
Moon HG, Han W, Ahn SK, Cho N, Moon WK, Im SA, et al. Breast cancer molecular phenotype and the use of HER2-targeted agents influence the accuracy of breast MRI after neoadjuvant chemotherapy. Ann Surg. 2013; 257:133-37.
Chen JH1, Bahri S, Mehta RS, Kuzucan A, Yu HJ, Carpenter PM, et al. Breast cancer: evaluation of response to neoadjuvant chemotherapy with 3.0-T MR imaging. Radiology. 2011; 261:735-43.
Chen JH, Agrawal G, Feig B, Baek HM, Carpenter PM, Mehta RS, et al. Triple-negative breast cancer: MRI features in 29 patients. Ann Oncol. 2007;18:2042-43.
Bufi E, Belli P, Di Matteo M, Terribile D, Franceschini G, Nardone L, et al. Effect of breast cancer phenotype on diagnostic performance of MRI in the prediction to response to neoadjuvant treatment. European Journal of Radiology.2014; 83:1631-38.
Park SH, Moon W, Cho N, Song IC, Chang JM, Park I-A, et al. Diffusion-weighted MR Imaging: pretreatment prediction of response to neoadjuvant chemotherapy in patients with breast cancer. Radiology.2010; 257:56-63.
Rieber A, Brambs HJ, Gabelmann A, Heilmann V, Kreienberg R, kühn T. Breast MRI for monitoring response ofprimary breast cancer to neo-adjuvant chemotherapy. Eur Radiol. 2002; 12:1711-9.
Denis F, Desbiez-Bourcier AV, Chapiron C, Arbion F, Body G, Brunereau L. Contrast enhanced magnetic resonance imaging underestimates residual disease following neoadjuvant docetaxel based chemotherapy for breast cancer. Eur J Surg Oncol. 2004;30:1069-7.
Honeth G, Bendahl PO, Ringnér M, Saal LH, Gruvberger-Saal SK, Lövgren K, et al. The CD44+/CD24- phenotype is enriched in basal-like breast tumors. Breast Cancer Res. 2008;10:R53.
Schwartz T, Stark A, Pang J, Awuah B, Kleer CG, Quayson S, et al. Expression of aldehyde dehydrogenasa 1 as a marker of mammary stem cells in benign and malignant breast lesions of Ghanaian women. Cancer. 2013;119:488-94.
Schmitz AMT, Loo CE, Wesseling J, Pijnappel RM, Gilhuijs KGA. Association between rim enhancement of breast cancer on dynamic contrast-enhanced MRI and patient outcome: impact of subtype. Breast Cancer Res Treat. 2014; 148:541-51.
Leek RD, Landers RJ, Harris AL, Lewis CE. Necrosis correlates with high vascular density and focal macrophage infiltration in invasive carcinoma of the breast. Br J Cancer 1999; 79:991-95.
Fisher ER, Anderson S, Redmond C, Fisher B. Pathologic findings from the national surgical adjuvant breast Project B-06:10 year pahtologic and clinical prognostic discriminants. Cancer 1993;71:2507-2514.
Jimenez RE, Wallis T, Visscher DW. Centrally necrotizing carcinoma of the breast: a distinct histologic sugtype with aggressive clinical behaviour. Am J Surg Pathol. 2001; 25:331-37.
Kawashima H, Inokuchi M, Furukawa H, Kitamura S. Triple-negative Breast Cancer: are the imaging findings different between responders and nonresponders to neoadyuvant chemotherapy? Acad Radiol. 2011; 18:963-969.
Kim JY, Kim SH, Kim YJ, Kang BJ, An BJ, Lee W, et al. Enhancement parameters on dynamic contrast enhanced breast MRI: do they correlate with prognostic factors and subtypes of breast cancers? Magnetic Resonace Imaging. 2015; 33:72-80.
Bae MS, Park SY, Song SE, Kim WH, Lee SH, Han W, et al. Heterogeneity of triple-negative breast cancer:mammographic, US,and MR imaging features according to androgen receptor expression. Eur Radiol. 2015; 25:419-27.
Agoff SN, Swanson PE, LindenH, Hawes SE, Lawton TJ. Androgen receptor expression in estrogen receptor-negative breast cancer: immunohistochemical, clinical, and prognostic associations. Am J Clin Pathol. 2013;120:725-31.
Kyndi M, Sorensen FB, Knudsen H, Overgaard M, Nielsen HM, Overgaard J, et al. Estrogen receptor, progesterone receptor, HER-2, and response to postmastectomy radiotherapy in high-risk breast cancer: the Danish Breast Cancer Cooperative Group. J Clin Oncol. 2008; 26:1419-26.